Overview of malignant pleural effusion.
 |
| malignant pleural effusion symptoms, causes and treatment. |
malignant pleural effusion It is a mixture involving the accumulation of fluids containing cancerous cells between the membranes lining the lungs.
It occurs in about 30% of lung cancers, but can also occur with other types of cancer, such as breast cancer, ovarian cancer, leukemia, and lymphoma.
With lung cancer, it may be malignant pleural effusion The first sign of cancer, or it can occur late in complications of advanced lung cancer.
What do you need to know about the symptoms, causes, and treatments of these infections?
Overview.
Known for malignant pleural effusion It is an abnormal amount of fluid in the vacuum between the layers of tissue (the sperm membrane) lining the lungs.
If cancer cells are present in this liquid (crystalline cavity), it is called malignant pleural effusion (Cancer) It may be malignant pleural effusion
Large, pervasive, or small and includes only a small portion of the pleural cavity.
The effusion may be in one area, or there may be many areas of leakage (inflated pleural effusion).
Reasons of malignant pleural effusion.
Almost any type of cancer can cause malignant pleural effusion if it is present in or spreads (metastasizes) to the chest area.
The most common are breast cancer, lung cancer, ovarian cancer, some types of leukemia, and lymphoma.
malignant pleural effusion may also be caused by treatments for lung cancer, such as surgery, radiotherapy, or chemotherapy.
Symptoms.
malignant pleural effusion symptoms can be very uncomfortable. Shortness of breath is one of the most common symptoms, occurring in about 80% of people.
Coughing may be present, and this is often topical, meaning it may be worse in certain situations such as leaning forward or lying on one side.
Chest compression or some types of abnormal chest sensation may also occur.
Diagnosis.
It is important to make an accurate diagnosis of malignant pleural effusion because the diagnosis and treatment are very different from a non-malignant pleural effusion (benign). It is important to note that even with cancer, up to 50 percent of pleural effusion is benign.
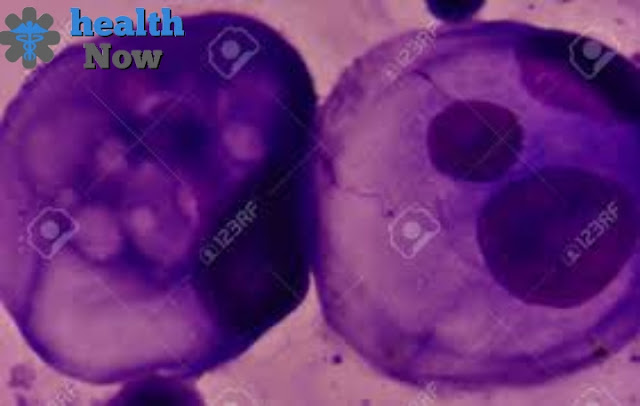
malignant pleural effusion is often first suspected due to symptoms or results on chest X-rays or CT scans. If your doctor suspects an eruption of malignant blueberries, the next step is usually a chest area, a process in which a needle is inserted through the chest wall into the pleural vacuum to obtain a sample of liquid. This liquid is then examined under a microscope to see if cancer cells exist.
If chest insolvency cannot be performed, or if the results are inconclusive, further procedures may be required to obtain an accurate diagnosis. In some cases, a chest endoscopy procedure (a procedure in which a chest endoscope is inserted into the chest) may be required to obtain a biopsy to diagnose malignant biliary.
Treatments of malignant pleural effusion.
The goal in the treatment of malignant pleural effusion is often analgesic, i.e. to improve quality of life and reduce symptoms but not to treat cancer.
Breaststroke.
As noted above, chest insolation is usually the first step used, to diagnose effusion (determine whether cancer cells are present in the liquid and more), and remove the liquid. Unfortunately, these distractions often come back.
For malignant pleural effusion that is repeated, there are several options for treating liquid and relieving shortness of breath.
At this time there is still considerable debate about the procedure that is better, often selected based on the severity of the symptoms, how the tumor responds to treatment, and the condition of your performance - about the extent of cancer interference with the ability to continue with normal daily activities.
Foreign adhesion.
One procedure that employs approximately 60 to 90 percent of people is called inflammation. In this procedure, the tube is inserted into the pleural space, and material, most commonly talc is inserted between the 2 membranes lining the lungs.
This chemical causes inflammation of the pleural cavity which in turn twists the whites together (valves) to prevent fluid from accumulating again in the pleural space.
Pleural Catheter.
Another procedure is a static pleural catheter, also known as a tunnel pleural catheter. In this procedure, a small tube is inserted into the pleural vacuum and subcutaneous tunnel, with a small hole on your side that can be covered with a bandage.
This allows patients to drain their fluids (with the help of a dear person) by attaching a vacuum container to open the skin.
Tunnel catheters are sometimes more effective if the bulge is on either side of the chest (binary) or if there are large areas of local fluid groups (perceptible bulge).
This procedure is often considered less attractive than dermatitis (Pleurodesis) and is effective in 80 percent to 100 percent of people.
Many researchers now feel that pleural catheterization (IPC) should be considered the first line in all people with malignant effusions.
There has been controversy over whether pneumonia (talc insertion) or Pacific membrane catheter residential is the best choice for people with advanced cancer and recurrent pleurisy.
The 2017 study published in JAMA, sought to answer this question. The researchers found that those who were resident tribal large catheters were less hospitalized than those with pleural, primarily associated with the need for procedures to remove the crystalline fluid.
Otherwise, there were no significant differences in the sense of shortness of breath or the quality of life of participants.
Additional treatment options.
If malignant pleural effusion persists Despite these other techniques, surgery can be performed to drain the liquid to the abdomen, or a pleural ablation can be performed (a procedure that removes part of the estrangement membrane).
New treatments (e.g. medical pleural endoscopy) appear to treat malignant pleural effusion too. Chemotherapy may help cause malignant crystal leukemia due to small cell lung cancer, but it is usually not very effective for those with non-small cell lung cancer.
Choose the best treatment.
Before it is recommended to use the crystalline membrane or pleural tunnel catheter, there are some necessary things.
First, your doctor will need to confirm that you have a malignant membrane effusion and that the symptoms are not due to another cause.
Secondly, you must have a pleuroscopy that repeats (returns) after thoracentesis. Most importantly, draining liquid from your pleural space should help treat symptoms of psychosocial distress.
It is not necessary to remove fluids just because they exist, but only if they cause problems (such as shortness of breath).
This is a very important point to repeat. If the cause of shortness of breath is caused by another underlying cause, and the removal of fluids will not make much difference, there is usually no benefit in removing the liquid.
Références.
Unfortunately, the life expectancy of lung cancer with malignant pleural effusion is less than 6 months. The average survival period (the time 50 percent of people died and 50 percent are still alive) is four months, although some people have stayed much longer.
Diagnosis is slightly better for those with malignant deep membrane leakage associated with breast or ovarian cancer in particular.
With the emergence of new treatments such as targeted therapies and immunotherapy, it is hoped that these numbers will change shortly.
There are also many clinical trials in progress in looking at the optimal treatment for these effusions.
Dealing with malignant pleural effusion.
The discomfort with malignant pleural effusion can be great. Pairing this with learning your diagnosis and misdiagnosis, the experience can be painful for anyone - especially those who already have malignant pleural effusion when they are first diagnosed with cancer.
Ask questions. Ask for help from others, and allow them to provide it. Talk to your doctor about managing pain from lung cancer.
Consider joining a support group. Your emotions may extend from the spectrum of anger to disbelief and depression. That's normal. Find friends and loved ones who are ready to listen and support you.
Read more:
What is the drug tagrisso - how it is used and what is damage.
What are small lymphocytic lymphoma-Specific treatments?
What is mesothelioma disease? Diagnosis and how it is treated.

